Most women leave their six-week postpartum visit with the same message: “You’re cleared.”
But being medically cleared doesn’t mean your body feels ready.
Leaking when you sneeze, a core that feels soft or unstable, a sense of heaviness “down there,” pain with intimacy, or anxiety about returning to exercise are all incredibly common after pregnancy and birth. They are also treatable. They’re not just “the new normal” you have to live with.
Postpartum pelvic floor physical therapy is designed to address exactly these issues. At Limitless Physical Therapy Specialists, we work with women in Victor, Brighton, and the surrounding Rochester area to help them understand what’s going on in their bodies and give them a clear, evidence-based path forward.
Why Postpartum Pelvic Floor Therapy Matters
Professional groups like ACOG now emphasize that postpartum recovery is a process, not a single appointment. They recommend that women begin gentle pelvic floor work in the early postpartum period and that those with higher-risk births receive closer follow-up and rehabilitation.
You may benefit from a pelvic floor assessment even more if you had a forceps or vacuum delivery, a long pushing phase, a large baby, or significant tearing or episiotomy. These situations put extra strain on the tissues and are associated with a higher risk of persistent symptoms like incontinence, prolapse, and pain.
The key idea is simple: pregnancy and childbirth change how your support system works. Your pelvic floor, abdominal wall, diaphragm, and deep stabilizing muscles don’t just get “tired”—their coordination and loading patterns are altered. Therapy helps restore that system instead of leaving you to guess your way through recovery.
What Pregnancy Actually Does to the Core and Pelvic Floor
During a vaginal delivery, the pelvic floor muscles can stretch to several times their resting length. Even when everything goes smoothly, that’s a significant mechanical and neurological load on the tissues.
Throughout pregnancy, hormones soften ligaments and connective tissue. Your posture shifts, your rib cage and diaphragm adapt to growing abdominal volume, and your abdominal wall gradually stretches to make room for your baby. After birth, many women show delayed activation and reduced strength in the pelvic floor and deep core, along with changes in spinal alignment and muscle balance around the hips and pelvis.
None of this means you’re “broken.” It simply means your body has gone through a major event, and like any other major musculoskeletal event, it responds best to structured rehabilitation instead of hope and time alone.
Common Postpartum Symptoms You Don’t Have to Live With
The research is consistent: pelvic floor and core-related symptoms are widespread after childbirth. A large share of women experience at least one of the following:
- Leaking urine with coughing, sneezing, laughing, running, or lifting
- A feeling of pressure, heaviness, or “something falling” in the vaginal area
- A visible or palpable abdominal separation (diastasis recti) or doming down the midline
- Pelvic, tailbone, hip, or low back pain that lingers beyond the immediate healing window
- Pain with intercourse or a sense of tension and guarding
It’s very common to be told, “That’s normal after a baby.” What the evidence says is more nuanced. These symptoms are common, but they are not inevitable, and they are not something you are required to tolerate. When addressed with targeted pelvic floor and core rehabilitation, they usually improve significantly.
The “Give It Time” Problem
Time alone doesn’t reliably close a significant diastasis, restore pelvic floor coordination, or resolve prolapse symptoms. Many studies show that a meaningful portion of women still have incontinence, separation, or pelvic pain a year or more after delivery if they do not receive treatment.
It’s also important to understand that Kegels are not a universal fix. Some women do in fact need strengthening. Others have a pelvic floor that is already overactive and tight, and adding more “squeezing” can actually worsen pain, urgency, or feelings of pressure. The first step is an assessment to understand what your system is doing, not a one-size-fits-all exercise.
What Postpartum Pelvic Floor Therapy Looks Like
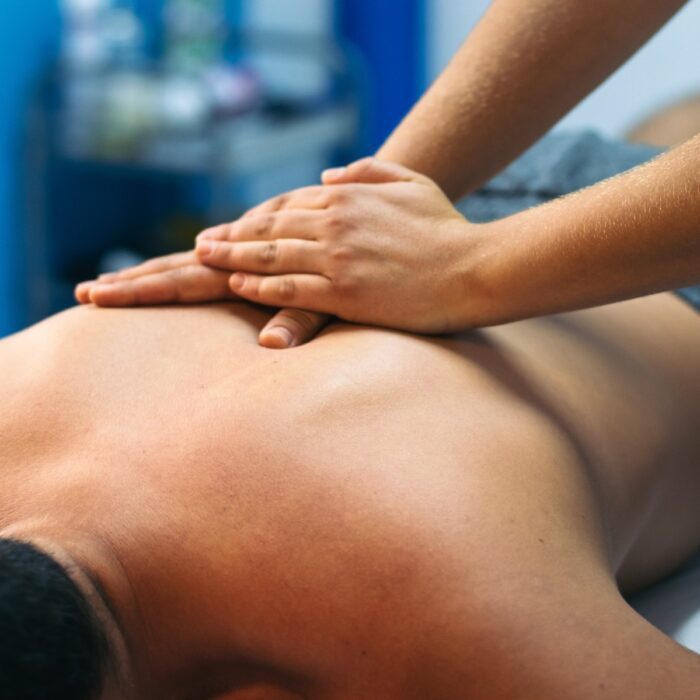
A pelvic floor physical therapy session is very different from a general postpartum workout or group fitness class. It starts with listening—your birth story, your symptoms, your activity level, and what you want to be able to do again.
From there, your therapist will typically look at:
- How your abdominal wall is healing, including any diastasis recti
- How your pelvic floor muscles contract, relax, and coordinate with your breath
- How your scars (cesarean or perineal) move and feel
- How your hips, spine, and rib cage are moving
- How you perform everyday tasks like lifting your baby, carrying a car seat, or getting up from the floor
Internal pelvic floor assessment is often recommended because it gives the clearest picture of muscle tone, strength, and coordination. It is always explained in advance and always your choice. Many women find it reassuring to have their symptoms finally examined in a focused, respectful way.
Treatment might include a blend of deep core retraining, pelvic floor strengthening or relaxation strategies, manual therapy to address scar tissue or muscle tension, work on breathing and pressure management, and gradual progression back into the activities you care about—whether that’s walking comfortably, returning to running, lifting weights, or simply going through the day without worrying about symptoms.
Diastasis, Incontinence, and Pelvic Pain: How Therapy Helps
For diastasis recti, the goal is not just “closing the gap,” but restoring tension and support across the abdominal wall. We focus on the transverse abdominis and its partners, teaching your core to turn on at the right time and in the right way. High-pressure movements like early sit-ups or aggressive planks are usually dialed back at first, then reintroduced strategically as your control improves.
For urinary incontinence, the treatment approach depends on what we find. If your pelvic floor is underactive, we build strength and endurance. If it’s overactive and guarded, we start with relaxation, mobility, and down-training before layering on more load. In both cases, coordination with breathing and movement is key.
For pelvic or tailbone pain, we look at the combination of scar mobility, joint mechanics, muscle tension, and nerve sensitivity. Manual therapy—both external and, when appropriate, internal—can be very helpful in restoring motion and comfort, but it is always paired with movement retraining so that gains carry over into your daily life.
Your Recovery Timeline
Every recovery is unique, but certain patterns show up again and again.
In the first six to eight weeks, the focus is on healing and gentle reactivation. This is when you start to reconnect with your core and pelvic floor, learn how to breathe in a way that supports healing, and begin to notice what does and doesn’t feel right.
From about two to six months postpartum, most women see their biggest changes if they are engaged in a structured rehab program. Strength, endurance, and confidence usually build steadily during this time. Leaking often decreases, abdominal control improves, and day-to-day movements feel more natural again.
Beyond six months, the emphasis often shifts to higher-level strength and impact. This might mean gradually returning to running, sports, lifting heavier weights, or other demanding activities. Having a therapist guide the timing and progression reduces the risk of flare-ups and setbacks.
Starting later doesn’t mean it’s “too late.” Women can and do make meaningful progress months or even years after childbirth when they finally get the right help.
How Limitless PT Supports Postpartum Women
At Limitless Physical Therapy Specialists, postpartum care is built around real life. We know you may be sleep-deprived, juggling feeding schedules, and unsure what your day will look like when you wake up.
That’s why sessions are individualized and flexible. You’re welcome to bring your baby. Your therapist will adjust the session based on how you feel that day—some visits will be more hands-on, others more focused on exercise and education. The goal is steady, sustainable progress, not perfection.
You’ll leave with a clear understanding of what’s happening in your body, what the next steps are, and how to tell if things are moving in the right direction.
Understanding Insurance and Access in New York
For many women, the biggest barrier to getting care is confusion about coverage. Fortunately, most major insurance plans do cover pelvic floor physical therapy when there are clear symptoms like incontinence, prolapse, pain, or diastasis. It is typically billed under outpatient physical therapy benefits.
New York is a direct-access state, which means you can see a physical therapist without a physician referral for a limited period (up to 10 visits or 30 days). Some insurers still prefer or require a referral for reimbursement, but this is usually a paperwork detail rather than a hard barrier.
At Limitless PT, our front desk team verifies your benefits before your first visit. We let you know if a referral is required, what your copay or coinsurance looks like, and whether there are any visit limits you should be aware of. If you don’t have coverage that fits your needs, we can discuss self-pay options as well.
From a cost perspective, pelvic floor therapy is also highly favorable. Research shows that conservative care resolves or greatly improves symptoms for most women and significantly reduces the likelihood of needing surgery for conditions like prolapse or incontinence. It’s a lower-risk, lower-cost, and often faster path back to function.
When You’re Ready to Start
You don’t have to wait until things feel “bad enough” to ask for help. If you’re noticing leaking, heaviness, abdominal bulging, pain, or just a sense that your body isn’t working the way it should after pregnancy, that’s a valid reason to be evaluated.
Limitless PT’s clinics in Victor and Brighton are equipped to support you through this season with compassionate, evidence-based postpartum care. Whether you are six weeks postpartum or several years out, you deserve a body that feels strong, supported, and trustworthy again.
When you’re ready, we’re here to help you take that next step.

![Arm Pain From Sleeping on Side: Causes and Fixes [PT Guide]](https://limitlesspts.com/wp-content/plugins/theplus_elementor_addon/assets/images/placeholder-grid.jpg)